Increased efficacy with increased dosage
REDUCTIONS IN MEAN WEEKLY RATE OF DROP SEIZURES (ATONIC, TONIC, OR MYOCLONIC) BY DOSE (N=217, mlTT)1,2
Study Design: CONTAIN (ClObazam in PatieNTs with Lennox-GAstaut SyNdrome) was a randomized, double-blind, placebo-controlled study consisting of a 4-week baseline period followed by a 3-week titration period and a 12-week maintenance period (N=238, randomized). Patients age 2 to 54 years with a current or prior diagnosis of LGS were stratified into 2 weight groups (12.5 kg to ≤30 kg or >30 kg), and then randomized to placebo or 1 of 3 target maintenance doses of ONFI. The dosage groups were: placebo (n=59); low-dose (5 mg/10 mg, n=58); medium-dose (10 mg/20 mg, n=62); and high-dose (20 mg/40 mg, n=59). Doses above 5 mg/day were administered in 2 divided doses. The primary endpoint was the percentage reduction in mean weekly rate of drop seizures (atonic, tonic, or myoclonic) from the 4-week baseline period to the 12-week maintenance period.
- Drop seizures were defined as drop attacks or spells that involved the entire body, trunk, or head, and1:
- Led to a fall or injury, slumping in a chair, or hitting the head on a surface
- Could have led to a fall or injury, depending on the position of the patient at the time of the attack or spell
- Patients in the trial experienced ≥2 drop seizures per week during the 4-week baseline period, while receiving stable doses of 1 to 3 antiepileptic drugs (AEDs) ≥30 days prior to screening1
- ONFI causes somnolence and sedation. In clinical trials, somnolence or sedation was reported at all effective doses and was dose-related. In general, somnolence and sedation begin within the first month of treatment and may diminish with continued treatment. Monitor patients for somnolence and sedation, particularly with concomitant use of other CNS depressants2
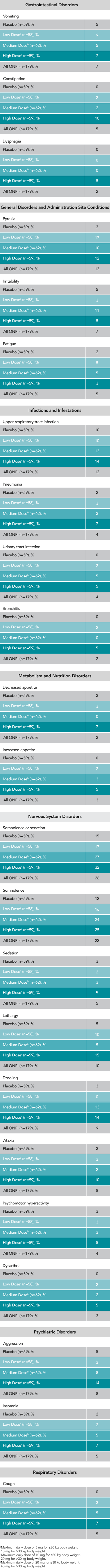
- Most common AEs (≥10% in any treatment group and ≥5% greater than placebo, respectively) were somnolence or sedation (32% vs. 15%), somnolence (25% vs. 12%), pyrexia (17% vs. 3%), lethargy (15% vs. 5%), aggression (14% vs. 5%), drooling (14% vs. 3%), irritability (11% vs. 5%), ataxia (10% vs. 3%), and constipation (10% vs. 0%)2
Key enrollment criteria1
- Age: 2 to 60 years
- LGS onset before 11 years of age
- Documentation of EEG with slow spike-and-wave (SSW) (<2.5 Hz) at some point in the patient's history
Safety Profile
ONFI safety results
ADVERSE REACTIONS REPORTED FOR ≥5% OF PATIENTS AND MORE FREQUENTLY THAN PLACEBO IN ANY TREATMENT GROUP1
Medical Information Inquiries
If you have a question or would like access to medical and scientific information regarding ONFI or any Lundbeck product, go to www. Lundbeckmedinfo.com where you can submit a medical question to the Lundbeck Medical Information support team.
References
- Ng YT, Conry JA, Drummond R, et al. Randomized, phase III study results of clobazam in Lennox-Gastaut syndrome. Neurology. 2011;77(15):1473-1481.
- ONFI [package insert]. Deerfield, IL: Lundbeck.
- Conry JA, Ng YT, Paolicchi JM, et al. Clobazam in the treatment of Lennox-Gastaut syndrome. Epilepsia. 2009;50(5):1158-1166.


